Triathlete Risk of Pelvic Floor Disorders, Pelvic Girdle Pain, and Female Athlete Triad Journal Article
Local Library Link: Find It @ Loyola
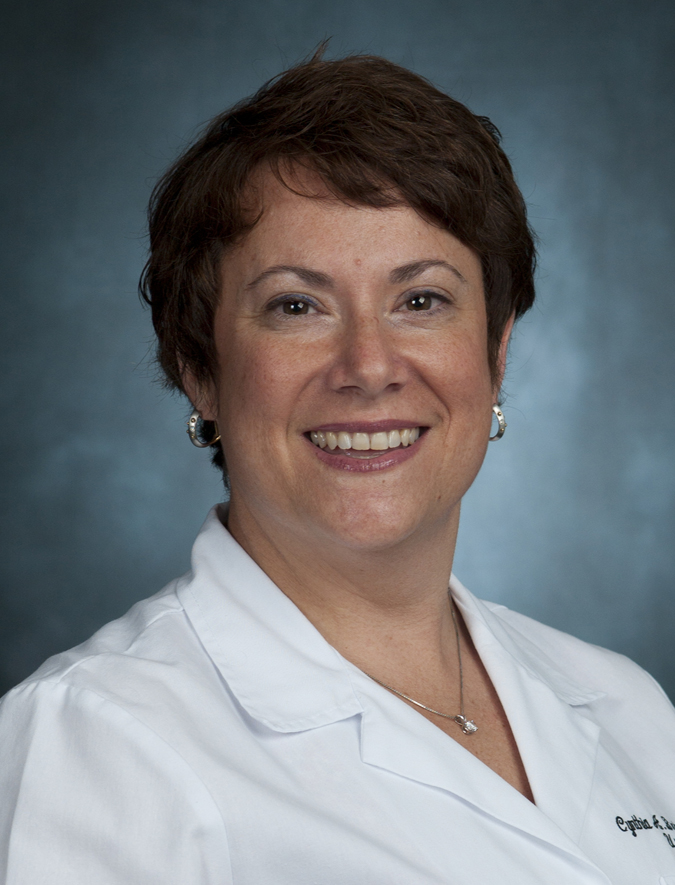
| Authors: | Yi, J; Tenfelde, S; Tell, D; Brincat, C; Fitzgerald, C. |
| Article Title: | Triathlete Risk of Pelvic Floor Disorders, Pelvic Girdle Pain, and Female Athlete Triad |
| Abstract: | OBJECTIVES: Our primary objective was to describe the prevalence of pelvic floor disorders (PFDs), pelvic girdle pain (PGP), and the female athlete triad (disordered eating, menstrual irregularities, and osteoporosis) in a female triathlete population. We also evaluated for an association between these conditions. METHODS: We administered an online survey to women who self-identified as female triathletes. Using validated questionnaires, Epidemiology of Prolapse and Incontinence Questionnaire and Pelvic Girdle Questionnaire, along with the female athlete triad questionnaire, we identified the prevalence of PFDs, PGP, and female athlete triad in this specific population. Demographic and exercise intensity were also queried to characterize these female triathletes. RESULTS: Three hundred eleven female triathletes responded to the Internet survey. There was a significant prevalence of PFDs with stress urinary incontinence and anal incontinence symptoms being most common (37.4% and 28%, respectively). Urgency urinary incontinence and pelvic organ prolapse were less common (16% and 5%, respectively). Stress urinary incontinence and pelvic organ prolapse were more common in parous triathletes (P = 0.001, P = 0.05). Pelvic girdle pain was noted in 18% of these triathletes but was not disabling. Twenty-four percent of participants screened positive for at least 1 arm of the female athlete triad. No association was found between the female athlete triad and PFDs. CONCLUSIONS: Pelvic floor disorders are common and bothersome in female triathletes. Pelvic girdle pain, while present, does not limit these athletes from their training. These female triathletes may be at risk for the female athlete triad. Female triathletes may be at risk for both metabolic and PFDs and should be screened when identified. |
| Journal Title: | Female Pelvic Medicine Reconstructive Surgery |
| ISSN: | 2151-8378 |
| Publisher: | Unknown |
| Date Published: | 2016 |
| Language: | ENG |
| DOI/URL: | |
| Notes: | LR: 20160728; JID: 101528690; aheadofprint |
LUC Authors
Related LUC Article